![canva-dried-maple-leaves-MADGyd5FMwQ[1]](https://www.lifestoryhub.com/wp-content/uploads/2019/11/canva-dried-maple-leaves-MADGyd5FMwQ1.jpg)
Useful practical links below. For those interested in the inexplicable and what may never end see my article ‘Out of Time’ in
Friends On The Shelf | independent literary magazine
A subject we don’t usually discuss is the process of dying, yet it such an intrinsic part of death and potentially the most frightening. I got to my 50’s without witnessing it directly. I had no idea that you stopped trying to feed or make someone drink in the days leading to death. If your loved person is old and in a residential establishment living with dementia, do look at the John’s Campaign website [scroll down for link]. It campaigns on how vital it is to have thought about wishes and feelings around illness in homes or hospitals and whether access is freely allowed to friends and relatives.
My father died in a care home last year. It was a good death and not just for him [we hoped] but for those around him. Part of the experience of a good death is connected to the environment someone is in. The term makes no sense unless you have lived through it and appreciate how a home and family can help this to happen. He suffered from Vascular Dementia and suddenly one day it was intuitively apparent to my family but not the staff, that he was dying. He had refused food for 24 hours and could not drink easily. We asked for a district nurse to be called out who confirmed that this was how the dying process can begin. The attitude of the medical practitioners who visited and the NHS leaflets they gave us [see link below] were invaluable in understanding the stages towards death and what relatives could do to help themselves and the dying person. In my father’s case it took five days. We were enormously grateful to be with him for this time.
Despite his power of attorney saying he did not want to die in hospital or be resuscitated, the agency manager was keen to call an ambulance but was dissuaded and therefore the trauma of an unnecessary hospital visit avoided. Our family were very clear, even putting up signs on walls clarifying the wishes of our father. From then on, family and friends were with our father almost continually and utmost respect to our needs was shown. It was beautiful sunny weather, so his windows were wide open on to the garden which had a soothing water feature trickling in the background. Fans for the heat were provided. The manager even stopped the gardener from his noisy strimming. Valuable time for the family was spent with my father playing his favourite music, reading poetry and doing lots of singing. We liked to think he enjoyed this and it certainly helped us to feel we could give something. Do see ideas around poetry and music in Poetry and Music section of this site. The staff were so sensitive; offering us refreshments and being present but not obtrusive. Our father needed no pain relief and went quietly during a half an hour gap when no one was with him. I am so grateful for the home’s flexibility on what appeared to be an unusual choice from a resident.
Avoidance of discussions around death can potentially make the experience when it comes, feel more complex than it nee ds to be. A campaign I support is Dignity in Dying
ds to be. A campaign I support is Dignity in Dying
Do watch Simon Boas’s two minutes on the subject below and note that in October 2024 his book comes out called ‘A beginners Guide to Dying’
A Beginner’s Guide to Dying by Simon Boas (youtube.com)
Do scroll down for further relevant links which seek to empower:
This is a book which examines our mortality and manages to be uplifting :
Do see this helpful link to NHS information on the last few hours and days of life:
https://www.nhs.uk/conditions/end-of-life-care/changes-in-the-last-hours-and-days/
See the site below which campaigns for access to friend’s and relatives for those not able to represent themselves:
This Age UK video is helpful for how to approach difficult conversations around death:
This is a very useful link useful to read for anyone thinking about quality at the end of their life. It explains about what a power of attorney is and what a living will is:
https://www.ageuk.org.uk/information-advice/money-legal/legal-issues/advance-decisions/
A power of attorney in relation to your health and care allows you to state what you want in relation to how you are treated at the end of your life [amongst other subjects which are explained] and is about the time when you may not have capacity to communicate this yourself. It involves other people who you put in a position to reflect your wishes if you are in a state of incapacitation.
A living will is written by you and expresses your wishes about your end of life care for when and if you don’t have capacity. You have full control of a living will and there is no need to involve a lawyer or anyone else. It is important you share a living will with those who are likely to be around you at the time of your death as it concerns your wishes about your end of life medical situation. The people to share it with could be family members or a GP or anyone else you trust.
Death cafes are further explained in this link; free ranging conversations about death for anyone interested with no agenda except to make it more comfortable to talk about. Possibly not suitable for those in the midst of intense grief or those nearing the end of life: What is Death Cafe
This site aims to support for anyone interested in accessing end of life support but a cost is usually associated with this:
Finally the government site to advise on what to do when someone has died:
What to do when someone dies: step by step – GOV.UK
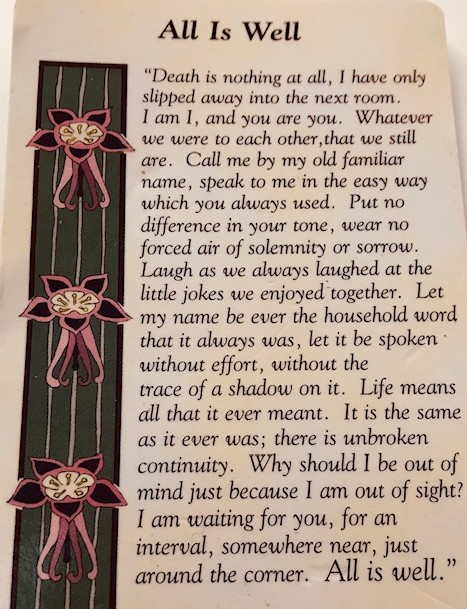
Henry Scott Holland’s words to pause on: